Latest Updates
-
 Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet
Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet -
 A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses
A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses -
 Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby
Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby -
 Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family
Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family -
 Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December -
 Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral
Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral -
 From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens
From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens -
 The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather
The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather -
 On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat
On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat -
 Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Meningococcal Meningitis Led To Two Deaths In Vietnam, Know The Causes, Symptoms, And Treatment
Two people in Vietnam's northern region have died of suspected meningococcal meningitis. Two other family members are hospitalised in critical condition, as reported by the National Tropical Disease Hospital on Wednesday, 12 June.
A 38-year-old male patient at the hospital's emergency department said his 22-month-old daughter and mother died within five days. They showed symptoms like high fever, headache, and diarrhoea, reported Xinhua news agency. Later, he and his 11-year-old son were diagnosed with meningococcal meningitis.
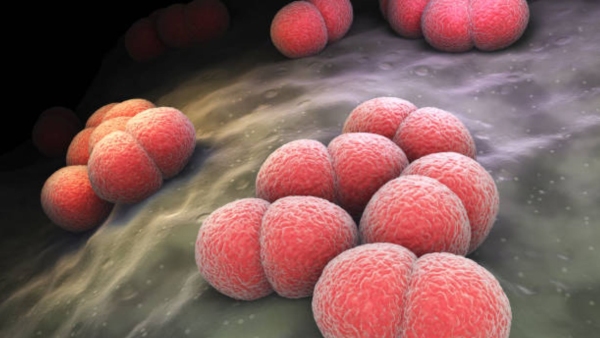
Through this post, let us know the causes, symptoms, risk factors, and treatment of meningococcal meningitis.
What Is Meningococcal Meningitis?
Meningococcal meningitis is a severe bacterial infection of the membranes covering the brain and spinal cord. It is a bacterial infection caused by Neisseria meningitidis, a pathogen known for its rapid progression and high mortality rate.
It primarily affects children, adolescents, and young adults but can occur in individuals of any age. The bacteria are spread through respiratory droplets, making close and prolonged contact a significant risk factor.
Meningococcal Meningitis: Causes
The primary cause of meningococcal meningitis is the bacterium Neisseria meningitidis. There are several serogroups of this bacterium, with A, B, C, W, X, and Y being the most common causes of outbreaks.
Neisseria meningitidis is transmitted through respiratory droplets from an infected person or asymptomatic carrier. Close and prolonged contact, such as living in close quarters, kissing, or sharing eating utensils, increases the risk of transmission. Outbreaks are more common in areas with dense populations, such as schools, military barracks, and dormitories.
Meningococcal Meningitis: Risk Factors
Several factors can increase the risk of contracting meningococcal meningitis, including:
- Age: Infants, children, and young adults are at higher risk.
- Living Conditions: Crowded environments facilitate the spread of the bacteria.
- Immunocompromised State: Individuals with weakened immune systems are more susceptible.
- Travel: Visiting areas where meningococcal meningitis is endemic increases risk.
- Medical Conditions: Certain conditions, such as spleen dysfunction, increase susceptibility.
Meningococcal Meningitis: Who Are At Risk?
Certain groups have a higher risk of contracting meningococcal disease. They include:
- Babies younger than one year
- Teenagers and young adults
- People visiting areas where the disease is prevalent
- Those with no spleen or an injured spleen
- Individuals with sickle cell disease
- People living in crowded places like college campuses or military barracks
- Laboratory workers exposed to the bacteria
Seeking immediate medical care is crucial. Early treatment of bacterial meningitis can prevent serious complications.
Meningococcal Meningitis: Symptoms
The symptoms of meningococcal meningitis can develop rapidly, often within hours of infection. Early symptoms may resemble those of the flu, which can delay diagnosis and treatment. Common symptoms include:
- Fever: Sudden onset of high fever
- Headache: Severe and persistent headache
- Stiff Neck: Neck stiffness and pain, making it difficult to touch the chin to the chest
- Nausea and Vomiting: Often accompanied by a poor appetite
- Photophobia: Sensitivity to light
- Altered Mental State: Confusion, drowsiness, and difficulty waking
- Rash: A distinctive purplish rash that does not blanch under pressure, indicating septicemia
In infants, the symptoms may be less specific and can include irritability, poor feeding, a bulging fontanel (soft spot on the head), and abnormal reflexes.
Meningococcal Meningitis: Diagnosis
Diagnosing meningococcal meningitis involves a combination of clinical evaluation and laboratory tests. Key diagnostic procedures include:
- Lumbar Puncture: A sample of cerebrospinal fluid (CSF) is collected and analyzed for the presence of bacteria.
- Blood Tests: Blood cultures can identify the bacteria in the bloodstream.
- Imaging: CT scans or MRIs may be used to rule out other conditions and assess complications.
Meningococcal
Meningitis:
Treatment
Immediate medical treatment is crucial for individuals with meningococcal meningitis. The primary goals of treatment are to eradicate the infection, manage symptoms, and prevent complications.
Antibiotic Therapy
Antibiotics are the cornerstone of meningococcal meningitis treatment. Empirical antibiotic therapy is often initiated before confirmation of the diagnosis due to the rapid progression of the disease. Commonly used antibiotics include:
- Penicillin: Effective against most strains of Neisseria meningitidis.
- Ceftriaxone or Cefotaxime: Broad-spectrum antibiotics used for initial treatment.
-
Chloramphenicol:
An
alternative
for
individuals
allergic
to
penicillin.
The choice of antibiotic may be adjusted based on the sensitivity profile of the isolated strain.
Supportive
Care
In addition to antibiotics, supportive care is essential to manage symptoms and complications. This may include:
- Intravenous Fluids: To maintain hydration and electrolyte balance.
- Oxygen Therapy: For patients with respiratory distress.
- Pain Relief: Analgesics to manage severe headache and muscle pain.
- Corticosteroids: To reduce inflammation and prevent neurological damage.
Preventive Measures
Prevention of meningococcal meningitis focuses on vaccination and prophylactic antibiotics for close contacts of infected individuals.
- Vaccination: Several vaccines are available to protect against different serogroups of Neisseria meningitidis. Routine vaccination is recommended for certain age groups and high-risk populations.
- Prophylactic Antibiotics: Close contacts of individuals with meningococcal meningitis may be given antibiotics such as rifampicin or ciprofloxacin to prevent infection.
Disclaimer: The information provided in this article is for general informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or a qualified healthcare provider with any questions you may have regarding a medical condition.



 Click it and Unblock the Notifications
Click it and Unblock the Notifications