Latest Updates
-
 Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby
Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby -
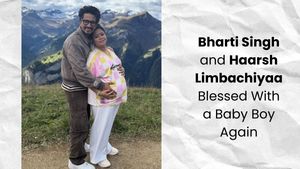 Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family
Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family -
 Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December -
 Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral
Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral -
 From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens
From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens -
 The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather
The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather -
 On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat
On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat -
 Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs -
 Paush Amavasya 2025: Do These Most Powerful Rituals For Closure On The Final Amavasya Of The Year
Paush Amavasya 2025: Do These Most Powerful Rituals For Closure On The Final Amavasya Of The Year -
 As The Last New Moon Of 2025 Approaches, Make A Wish Based On Your Rising Sign
As The Last New Moon Of 2025 Approaches, Make A Wish Based On Your Rising Sign
Kerala Teen Falls Victim To Deadly Brain-Eating Amoeba, Everything You Need To Know About This Disease
A 12-year-old boy named E.P Mridul from Feroke, Kerala passed away on 04 July after battling primary amoebic meningoencephalitis at a private hospital in Kozhikode. This marks the third fatality from this rare infection in Kerala within two months.
Mridul, a Class VII student at Farook Higher Secondary School, initially sought treatment for headache and vomiting at the government taluk hospital in Feroke last month. He had bathed in a local pond near Farook College before his symptoms began. His condition worsened, leading to his transfer to the Government Medical College Hospital in Kozhikode and then to a private hospital.

Recent Cases of Brain-Eating Amoeba
On
June
12,
V.
Dakshina,
a
13-year-old
from
Kannur,
succumbed
to
the
same
infection
at
a
private
hospital
in
Kozhikode.
Earlier,
on
May
20,
Fadva,
a
5-year-old
from
Munniyur
in
Malappuram,
died
at
the
Government
Medical
College
Hospital
in
Kozhikode
due
to
this
infection.
Know
more
about
this
deadly
brain
What Is Primary Amoebic Meningoencephalitis (PAM)?
Primary Amoebic Meningoencephalitis (PAM) is a severe and often fatal brain infection caused by the free-living amoeba Naegleria fowleri. This amoeba is commonly found in warm freshwater environments such as lakes, rivers, and hot springs. The infection occurs when contaminated water enters the body through the nose, leading to a rapidly progressing disease that affects the central nervous system (CNS).
The Causative Agent: Naegleria fowleri
Naegleria fowleri is an amoeba, a single-celled organism, that thrives in warm freshwater environments. It is thermophilic, meaning it prefers warm temperatures, typically between 25°C and 45°C (77°F and 113°F), but can survive at higher temperatures. Naegleria fowleri can exist in three different forms:
1. Trophozoite: This is the feeding and reproductive stage of the amoeba, where it actively moves and consumes bacteria and other organic material.
2. Flagellate: In unfavorable conditions, such as a lack of food, the trophozoite can transform into a flagellate form, which has two flagella and can swim in water.
3. Cyst: When environmental conditions become harsh, Naegleria fowleri can encyst, forming a protective wall around itself to survive until conditions improve.
Primary Amoebic Meningoencephalitis (PAM) Symptoms
The symptoms of amoebic meningoencephalitis can vary depending on the causative agent but often progress rapidly and can be severe:
Stage 1: Early symptoms typically appear 1 to 9 days after exposure and may include headache, fever, nausea, vomiting, and a stiff neck.
Stage 2: As the infection progresses, symptoms can escalate to confusion, lack of attention to people and surroundings, loss of balance, seizures, hallucinations, and eventually coma. The disease progresses rapidly and can lead to death within 1 to 18 days after symptoms begin.
Primary Amoebic Meningoencephalitis (PAM) Risk Factors
Several risk factors can increase the likelihood of contracting amoebic meningoencephalitis:
1. Exposure to Warm Freshwater: Activities like swimming, diving, or playing in warm freshwater lakes and rivers can increase the risk of exposure to Naegleria fowleri.
2. Use of Contaminated Water: Using untreated or poorly treated water for nasal irrigation or religious practices can introduce amoebae into the nasal passages.
3. Compromised Immune System: Individuals with weakened immune systems, including those with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive drugs, are at higher risk for GAE.
4. Soil Contact: Exposure to soil or dust, especially in areas where Acanthamoeba or Balamuthia are present, can increase the risk of infection.
Primary Amoebic Meningoencephalitis (PAM) Precautions
Preventing amoebic meningoencephalitis involves reducing exposure to the causative amoebae.
1. Avoid Water Activities in Warm Freshwater: Refrain from swimming or diving in warm freshwater lakes, rivers, and hot springs, especially during periods of high water temperature.
2. Use Safe Water for Nasal Irrigation: Use only sterile, distilled, or previously boiled water for nasal rinses and other activities that introduce water into the nasal passages.
3. Proper Pool Maintenance: Ensure that swimming pools and hot tubs are adequately chlorinated and maintained to prevent the growth of Naegleria fowleri.
4. Use Nose Clips: Wearing nose clips while swimming, diving, or participating in water activities can help prevent water from entering the nasal passages.
5. Avoid Stirring Up Sediment: Avoid disturbing the sediment in warm freshwater bodies where the amoeba may reside.
6. Use Nose Clips: When engaging in freshwater activities, use nose clips to prevent water from entering the nasal passages.
7. Avoid Soil Contact: Limit exposure to soil and dust, especially in areas known to harbor Acanthamoeba or Balamuthia.
Primary Amoebic Meningoencephalitis (PAM) Diagnosis
Diagnosing PAM is challenging due to its rarity and the similarity of its symptoms to bacterial meningitis. Key diagnostic methods include:
Lumbar
Puncture
(Spinal
Tap):
This
procedure
is
used
to
collect
cerebrospinal
fluid
(CSF)
for
testing.
The
presence
of
Naegleria
fowleri
can
be
confirmed
through
microscopic
examination,
culture,
or
polymerase
chain
reaction
(PCR)
testing
of
the
CSF.
Imaging
Studies:
MRI
or
CT
scans
of
the
brain
may
show
swelling
and
other
abnormalities,
but
these
are
not
specific
to
PAM.
Autopsy:
In
fatal
cases,
an
autopsy
may
be
performed
to
definitively
identify
the
presence
of
the
amoeba
in
brain
tissue.
Primary Amoebic Meningoencephalitis (PAM) Prognosis
The prognosis for PAM is generally poor. The disease progresses rapidly, and the majority of cases result in death within a few days to weeks after the onset of symptoms. Early diagnosis and aggressive treatment are crucial for any chance of survival, but even with prompt medical intervention, the survival rate remains low.
Only a few documented cases of survival exist, often involving early diagnosis, aggressive treatment, and possibly the use of experimental therapies.
Primary Amoebic Meningoencephalitis (PAM) Treatment
Treating PAM is exceptionally challenging due to the rapid progression and high mortality rate of the disease. Early diagnosis and prompt treatment are critical:
Antimicrobial Therapy
- Amphotericin B: This antifungal medication is the primary drug used to treat PAM. It can be administered intravenously or directly into the brain (intrathecally).
- Rifampin: An antibiotic that may be used in combination with other drugs.
- Fluconazole and Azithromycin: These antifungal and antibiotic medications are often included in treatment regimens.
- Miltefosine: An investigational drug that has shown some promise in treating PAM, used in combination with other medications.
Therapeutic
Hypothermia
Lowering
the
body
temperature
to
reduce
brain
swelling
and
metabolic
demands
has
been
used
as
an
adjunctive
treatment
in
some
cases.
Therefore, it is only through public awareness and education on the risks associated with this disease are essential for preventing this deadly infection.
Disclaimer: The information provided in this article is for general informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or a qualified healthcare provider with any questions you may have regarding a medical condition.



 Click it and Unblock the Notifications
Click it and Unblock the Notifications