Latest Updates
-
 Sreenivasan Passes Away: Malayalam Cinema Mourns The Legendary Actor-Writer's Demise
Sreenivasan Passes Away: Malayalam Cinema Mourns The Legendary Actor-Writer's Demise -
 Malayalam Film Industry Loses A Defining Voice: Actor, Screenwriter And Director Sreenivasan Passes Away At 69
Malayalam Film Industry Loses A Defining Voice: Actor, Screenwriter And Director Sreenivasan Passes Away At 69 -
 Happy Birthday Dheeraj Dhoopar: How A TV Set Friendship Turned Into Love With Wife Vinny Arora
Happy Birthday Dheeraj Dhoopar: How A TV Set Friendship Turned Into Love With Wife Vinny Arora -
 Top Skin and Hair Concerns in India in 2025: What the Data Reveals
Top Skin and Hair Concerns in India in 2025: What the Data Reveals -
 International Human Solidarity Day 2025: History, Significance, and Why It Matters
International Human Solidarity Day 2025: History, Significance, and Why It Matters -
 Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet
Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet -
 A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses
A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses -
 Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby
Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby -
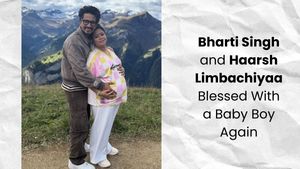 Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family
Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family -
 Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
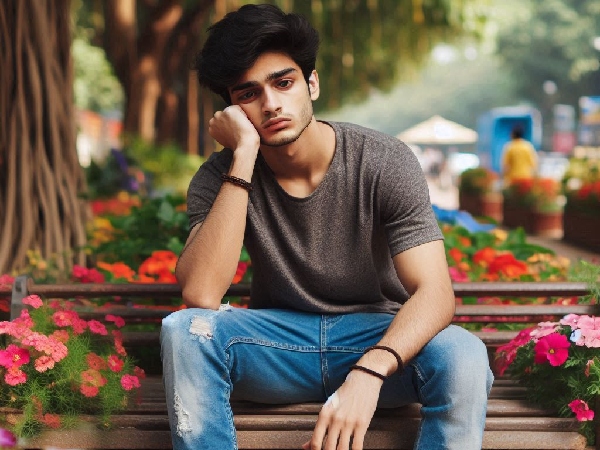
Feeling Down? Here’s The Surprising Connection Between Your Gut Health and Mood
We all have those days when we feel off, whether it's waking up in a bad mood or struggling to shake off a feeling of anxiety. It's easy to blame stress, lack of sleep, or just a rough day, but what if the answer lies deeper, inside us? A study shows that the key to our mood might not just be in our brain, but also in something much less obvious, our gut. Yes, your stomach could be the unexpected culprit or hero when it comes to how you feel. Let's find out how.
The Link Between Gut Microbes And Brain Health
A research has delved into the surprising link between our gut microbes and brain health, especially when it comes to depression. This study involving two large European groups discovered that people with depression seem to lack certain types of gut bacteria.
While it's unclear whether this missing bacteria is the cause or a result of depression, scientists found that these microbes can produce chemicals that might influence how our brain cells work and potentially affect our mood.
John Cryan, a neuroscientist who's been a big advocate of the gut-brain connection, sees this as a groundbreaking step forward, moving beyond small studies and animal tests.
There's even buzz around new treatments, like faecal transplants, where researchers are exploring whether altering the gut microbiome could help those battling depression. It's a fascinating area of study that's gaining real momentum!
A Gut Feeling
Several studies in mice have shown that gut microbes can influence behaviour, and small studies in humans hinted that depression might come with changes in the microbial balance. To explore this connection on a larger scale, Jeroen Raes, a microbiologist at the Catholic University of Leuven in Belgium, and his team studied the microbiomes of 1054 Belgians to establish a "normal" baseline.
Out of this group, 173 participants had been diagnosed with depression or scored poorly on a quality of life survey. The researchers found that two specific microbes Coprococcus and Dialister were missing from the microbiomes of people with depression, but were present in those with better quality of life.
This result held true even after considering factors like age, sex, and antidepressant use. Additionally, the researchers noted that people with depression had higher levels of bacteria linked to Crohn's disease, which points to possible inflammation being a factor. This study, published in Nature Microbiology in 2019, provides substantial evidence to support the growing understanding of how gut health can influence mental well-being
Missing Microbes And Depression
Researchers, led by Jeroen Raes, looked at the microbiomes of people with depression in two large groups-one Belgian and one Dutch. In both groups, they found that two specific microbes, Coprococcus and Dialister, were missing in people with depression, including those with severe depression. This finding suggests a possible link between these microbes and depression.
The team also explored how these microbes might affect mood. They identified 56 substances that gut microbes either produce or break down, which are important for the nervous system. They discovered that Coprococcus is involved in producing dopamine (a brain chemical linked to mood) and butyrate (an anti-inflammatory substance). Since inflammation is often connected to depression, these microbes could play a role in regulating mood.
Though the study doesn't prove that missing microbes cause depression, it offers strong evidence, backed by data from three different groups, that gut health may influence mental well-being.
However, the exact mechanism behind how these microbial compounds affect the brain is still unclear. One potential pathway is the vagus nerve, which connects the gut and the brain, acting as a possible communication channel for these microbes' effects on mental health.
Microbiome Profiling
Raes suggests that understanding the microbiome-brain connection could lead to new therapies for depression. Some doctors and companies are already exploring probiotics as a treatment, though they don't usually focus on the specific missing microbes identified in the study.
André Schmidt, a clinical neuroscientist, is conducting a trial where 40 depressed participants undergo faecal transplants to see if altering their microbiome affects their mental health. While more studies are needed, Sven Pettersson, a biologist who first suggested the link between the microbiome and mental health, believes these findings are a "massive signal" for doctors to consider microbiome profiling in their treatment of depression.
Turns out, the key to feeling better might be closer than you think-right in your gut! As science uncovers more about the gut-mood connection, it's clear that taking care of your microbiome could be a game changer for your mental well-being. So, maybe it's time to listen to your gut, after all!
Disclaimer: The information provided in this article is for general informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or a qualified healthcare provider with any questions you may have regarding a medical condition.



 Click it and Unblock the Notifications
Click it and Unblock the Notifications