Latest Updates
-
 Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet
Purported Video of Muslim Mob Lynching & Hanging Hindu Youth In Bangladesh Shocks Internet -
 A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses
A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses -
 Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby
Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby -
 Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family
Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family -
 Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December -
 Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral
Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral -
 From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens
From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens -
 The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather
The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather -
 On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat
On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat -
 Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Mad Cow-Like Illness Kills US Woman After 50-Year Dormancy, Know What It Is, How It Stayed Quiet For 50 Years
In an astonishing medical case, a woman succumbed to a fatal prion disease, marking potentially the longest incubation period for such a condition ever recorded.
This case, highlighted in the journal Emerging Infectious Diseases, involved a 58-year-old who developed Creutzfeldt-Jakob disease (CJD) approximately five decades after receiving contaminated human growth hormone (HGH) treatments as a child. The incident underscores the perplexing and often insidious nature of prion diseases, which can lie dormant for years before manifesting.
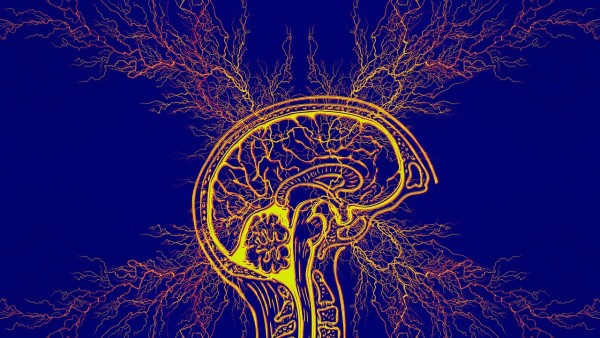
Prion diseases, including CJD, are caused by the abnormal folding of normal prion proteins in the brain, leading to a cascade of neurodegenerative effects. These conditions are notoriously difficult to prevent or cure, given prions' resistance to conventional sterilization methods that effectively neutralize other pathogens. While prion diseases are exceptionally rare, their impact is devastating, often resulting in rapid cognitive decline and death shortly after symptoms emerge.
The unfortunate death of the woman, who first presented with tremors and balance issues, rapidly deteriorated into a comatose state from which she never recovered. Her autopsy confirmed CJD without any genetic predispositions, pointing to her childhood HGH treatments as the likely source. This revelation is alarming, as it suggests that prion diseases can incubate for an extended period, in this case, potentially over 50 years, before showing any clinical signs.
Medical History And The Spread Of Prion Diseases
Historically, CJD and other prion diseases have been transmitted through various means, including consumption of infected beef and medical treatments like HGH derived from human cadavers. The latter practice was ceased in the U.S. and other countries following the discovery of its link to CJD, shifting towards synthetic alternatives. Despite this change, over two hundred cases of iatrogenic CJD, resulting from medical intervention, have been documented globally, with most cases emerging within a decade of treatment. However, as evidenced by this report, the latency period can extend much longer.
The U.S. altered its HGH extraction method in 1977, significantly reducing the risk of prion contamination. Nonetheless, the woman's initial and final treatments spanned from 51.3 years to 42.1 years before symptom onset, with a probable infection timeline estimated at about 48.3 years prior. This case, therefore, not only sets a record for the latency period of HGH-related CJD but also raises concerns about potential future cases. Individuals who received HGH before the 1977 method change remain at risk.
The presence of genetic factors can influence one's susceptibility to prion diseases, as the woman in question had a genetic mutation associated with prolonged latency periods. This suggests that while the incidence of CJD due to contaminated HGH has dramatically declined, the risk persists for some, notably those treated before 1977. Researchers estimate that around 7,700 people in the U.S. received HGH treatments before the implementation of safer practices, indicating a need for continued vigilance.
Let
us
know
more
about
Creutzfeldt-Jakob
disease
(CJD)
and
the
causes,
symptoms,
precautions
and
treatments
associated
with
it.
Creutzfeldt-Jakob
Disease
(CJD)
is
a
rare,
fatal
neurodegenerative
disorder
that
has
puzzled
scientists
and
clinicians
for
decades.
Often
likened
to
"mad
cow
disease" in
humans,
CJD
is
caused
by
misfolded
proteins
known
as
prions,
which
lead
to
rapid
brain
deterioration.
Despite
its
rarity,
the
disease's
swift
progression
and
lack
of
effective
treatment
make
it
a
significant
concern
in
neurology
and
public
health.
CJD
is
part
of
a
group
of
diseases
called
transmissible
spongiform
encephalopathies
(TSEs),
characterized
by
sponge-like
changes
in
brain
tissue.
The
disease
manifests
in
several
forms:
- Sporadic CJD (sCJD): Accounts for approximately 85% of cases and arises spontaneously without known cause.
- Familial CJD (fCJD): Inherited through mutations in the PRNP gene, representing about 10-15% of cases.
- Iatrogenic CJD: Results from exposure to contaminated medical equipment or procedures, such as corneal transplants or hormone treatments.
- Variant CJD (vCJD): Linked to consuming beef products infected with bovine spongiform encephalopathy (BSE), commonly known as mad cow disease.
CJD Causes And Transmission
The
primary
culprit
in
CJD
is
the
prion
protein,
which,
when
misfolded,
induces
other
normal
prion
proteins
to
also
misfold,
leading
to
a
chain
reaction
of
brain
damage.
Unlike
bacteria
or
viruses,
prions
lack
nucleic
acids,
making
them
resistant
to
standard
sterilization
processes.
Transmission
can
occur
through:
- Genetic inheritance: Mutations in the PRNP gene can be passed down, leading to familial CJD.
- Contaminated medical procedures: Use of infected surgical instruments or biological products.
- Consumption of infected meat: Particularly in cases of vCJD linked to BSE-infected beef.
CJD Symptoms And Progression
CJD
is
notorious
for
its
rapid
progression.
Initial
symptoms
often
include:
Cognitive
decline:
Memory
loss,
confusion,
and
impaired
judgment.
Behavioral
changes:
Personality
shifts,
anxiety,
and
depression.
Physical
symptoms:
Muscle
stiffness,
involuntary
movements
(myoclonus),
and
coordination
problems.
As the disease advances, patients may experience severe dementia, blindness, and eventually lapse into a coma. The median survival time after symptom onset is approximately one year.
CJD Diagnosis
Diagnosing
CJD
involves
a
combination
of
clinical
evaluation
and
specialized
tests:
Electroencephalogram
(EEG):
Detects
characteristic
brain
wave
patterns
associated
with
CJD.
Magnetic
Resonance
Imaging
(MRI):
Identifies
specific
changes
in
brain
tissue.
Cerebrospinal
fluid
tests:
Detects
proteins
indicative
of
prion
disease.
Definitive diagnosis often requires brain tissue examination, typically post-mortem.
CJD Treatment And Management
Currently,
there
is
no
cure
for
CJD.
Treatment
focuses
on
alleviating
symptoms
and
providing
supportive
care:
Medications:
Sedatives
and
antidepressants
can
help
manage
psychological
symptoms,
while
drugs
like
clonazepam
may
reduce
muscle
jerks.
Palliative
care:
Ensures
patient
comfort,
addressing
pain
and
other
distressing
symptoms.
CJD Precautions and Prevention
Preventing
CJD
involves
stringent
measures,
especially
in
medical
settings:
Sterilization
protocols:
Ensuring
surgical
instruments
are
properly
sterilized
to
eliminate
prion
contamination.
Screening:
Careful
screening
of
blood
and
tissue
donors
to
prevent
iatrogenic
transmission.
Food
safety:
Regulations
to
prevent
BSE-infected
meat
from
entering
the
food
supply
have
significantly
reduced
vCJD
cases.
Disclaimer: The information provided in this article is for general informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or a qualified healthcare provider with any questions you may have regarding a medical condition.



 Click it and Unblock the Notifications
Click it and Unblock the Notifications