Latest Updates
-
 A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses
A Hotel on Wheels: Bihar Rolls Out Its First Luxury Caravan Buses -
 Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby
Bharti Singh-Haarsh Limbachiyaa Welcome Second Child, Gender: Couple Welcome Their Second Baby, Duo Overjoyed - Report | Bharti Singh Gives Birth To Second Baby Boy | Gender Of Bharti Singh Haarsh Limbachiyaa Second Baby -
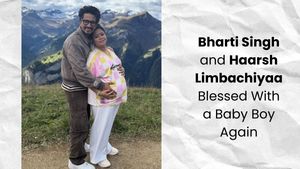 Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family
Bharti Singh Welcomes Second Son: Joyous News for the Comedian and Her Family -
 Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December
Gold & Silver Rates Today in India: 22K, 24K, 18K & MCX Prices Fall After Continuous Rally; Check Latest Gold Rates in Chennai, Mumbai, Bangalore, Hyderabad, Ahmedabad & Other Cities on 19 December -
 Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral
Nick Jonas Dancing to Dhurandhar’s “Shararat” Song Goes Viral -
 From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens
From Consciousness To Cosmos: Understanding Reality Through The Vedic Lens -
 The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather
The Sunscreen Confusion: Expert Explains How to Choose What Actually Works in Indian Weather -
 On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat
On Goa Liberation Day 2025, A Look At How Freedom Shaped Goa Into A Celebrity-Favourite Retreat -
 Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs
Daily Horoscope, Dec 19, 2025: Libra to Pisces; Astrological Prediction for all Zodiac Signs -
 Paush Amavasya 2025: Do These Most Powerful Rituals For Closure On The Final Amavasya Of The Year
Paush Amavasya 2025: Do These Most Powerful Rituals For Closure On The Final Amavasya Of The Year
Feeling Low? How Depression Messes With Your Menstrual Cycle, According To Science
Mental health and physical health are deeply connected, yet we often treat them like two separate issues. One place where this disconnect becomes painfully clear is the menstrual cycle.
For many people assigned female at birth, the monthly rhythm of hormones doesn't just influence their physical body - it's also closely tied to their emotional and mental well-being. But what happens when depression enters the picture?

Depression is more than feeling sad. It's a clinical mental health condition that affects every part of life - energy, appetite, sleep, focus, and yes, even periods. If your menstrual cycle has become irregular, heavier, lighter, more painful, or even absent altogether, and you're also struggling with depression, the two could be more connected than you think.
Let's understand the deep, complex relationship between depression and the menstrual cycle - how one affects the other, what the science says, and how to manage this challenging overlap with knowledge, compassion, and proactive care.
How The Menstrual Cycle Works
Before knowing how depression interferes, it's helpful to understand how a healthy menstrual cycle functions. A typical menstrual cycle lasts between 21 and 35 days and is regulated by a symphony of hormones - mainly estrogen and progesterone, with the pituitary gland releasing follicle-stimulating hormone (FSH) and luteinizing hormone (LH) to drive the process.
During the first half of the cycle (the follicular phase), estrogen rises to prepare the body for ovulation. After ovulation, the luteal phase begins, where progesterone dominates. If pregnancy doesn't occur, hormone levels fall, triggering menstruation.
This cycle is governed by the hypothalamic-pituitary-ovarian (HPO) axis, which is sensitive to stress, emotions, and physical health. When depression disrupts the brain's regulation of this axis, the menstrual cycle can get thrown off in a variety of ways.
Depression's Impact On Hormonal Balance
Depression
alters
the
balance
of
neurotransmitters
in
the
brain,
particularly
serotonin,
dopamine,
and
norepinephrine
-
chemicals
that
also
interact
with
reproductive
hormones.
Research
shows
that
serotonin,
which
helps
regulate
mood,
also
plays
a
role
in
modulating
the
HPO
axis.
When
serotonin
levels
are
low,
as
in
many
cases
of
depression,
this
can
interfere
with
the
release
of
FSH
and
LH
from
the
pituitary
gland.
That
disruption
can
delay
or
completely
prevent
ovulation.
Estrogen also affects serotonin levels, which may explain why some women report feeling more depressed right before their period - a time when estrogen dips dramatically. It's a two-way street: depression affects hormonal balance, and hormonal changes influence mood.
Moreover, cortisol - the primary stress hormone - is elevated in many people with depression. High cortisol can suppress reproductive hormones, particularly gonadotropin-releasing hormone (GnRH), leading to irregular or missed periods.
Irregular Periods And Missed Cycles
One of the most common menstrual symptoms linked to depression is irregularity. Women with clinical depression are more likely to report cycles that are shorter, longer, unpredictable, or absent. Amenorrhea (the absence of menstruation) can result from severe chronic depression, especially when accompanied by significant weight loss, low appetite, or intense stress.
This irregularity can be distressing on its own, but it's also a sign that the body is under strain. Depression often causes disruptions in sleep, appetite, physical activity, and overall health - all of which can contribute to menstrual disturbances.
Studies show that people with major depressive disorder are at increased risk of developing secondary amenorrhea (losing their period after having normal cycles previously), particularly if their depression is untreated or severe. Adolescents and young adults are especially vulnerable, as their reproductive systems are still maturing and more sensitive to environmental and emotional stressors.
Worsened Premenstrual Symptoms
People with depression often experience more intense premenstrual symptoms (PMS) or even premenstrual dysphoric disorder (PMDD) - a severe form of PMS marked by extreme mood changes, irritability, and fatigue. The week or two before menstruation can feel like an emotional avalanche, where depressive symptoms worsen, only to slightly ease up after menstruation begins.
This heightened sensitivity is due to how fluctuating hormones interact with mood-regulating brain chemicals. Those who already struggle with depression may find that normal hormonal shifts hit harder, triggering deeper lows, tearfulness, or hopelessness right before their period.
This cycle can become self-reinforcing - worsening mood leads to more hormonal instability, which worsens menstrual symptoms, and so on. It's no surprise that many report feeling emotionally trapped in the ups and downs of each month.
Menstrual Pain And Depression: A Physical-Mental Loop
Depression is associated with heightened pain sensitivity, meaning cramps and other menstrual discomforts can feel more intense. Conversely, experiencing chronic or severe menstrual pain can worsen depressive symptoms. This can lead to a vicious cycle where physical discomfort and emotional distress amplify one another.
For some, dysmenorrhea (painful periods) becomes more debilitating in the presence of depression. They may experience lower pain thresholds, increased fatigue, and lower motivation to manage the pain through exercise, warm compresses, or medication.
Furthermore, people with depression often find it harder to advocate for themselves medically. They may delay gynecological checkups or dismiss their symptoms as "just in their head," even when the pain is real and treatable.
Role of Antidepressants and Medications
It's worth noting that certain medications used to treat depression can also influence the menstrual cycle. Selective serotonin reuptake inhibitors (SSRIs), while highly effective for mood symptoms, can sometimes cause changes in cycle length, flow, or timing.
On the flip side, antidepressants can also help regulate cycles when depression is the underlying cause of hormonal disruption. By stabilizing mood and reducing cortisol levels, medication can support the return of regular ovulation and menstruation.
It's important to discuss any menstrual changes with both your psychiatrist and gynecologist. Sometimes adjusting the dose or switching medications can help find a better balance between emotional and physical well-being.
Managing Depression And Menstrual Health Together
The first step toward managing both depression and menstrual issues is to take them seriously - neither is "just a bad mood" or "just a bad period." They're interconnected medical conditions that deserve attention, support, and holistic care.
Regular mental health therapy, especially cognitive behavioral therapy (CBT), has been shown to improve mood and reduce PMS and PMDD symptoms. Mindfulness practices, exercise, and a diet rich in omega-3s, B vitamins, and iron can also support hormone balance and emotional stability.
Tracking your menstrual cycle alongside your mood can be a powerful tool. Many period tracking apps now include mental health logs, allowing you to spot patterns and plan ahead. If you notice consistent mood dips before your period or worsening depression during specific phases of your cycle, share this with your healthcare provider.
In some cases, hormonal treatments like birth control pills or hormonal IUDs may help stabilize the menstrual cycle and reduce severe premenstrual mood swings. These should be considered carefully and individually, particularly in those with a history of mood disorders, as hormonal contraception can sometimes affect mood in unexpected ways.
You're Not Imagining It - And You're Not Alone
If you've felt like your body is out of sync with your emotions, or your periods have become unpredictable or painful alongside your depression, know that you're not alone - and you're not imagining it. Depression and the menstrual cycle are deeply interwoven, affecting each other in complex and powerful ways.
The key lies in understanding the connection, advocating for integrated care, and giving yourself grace. Healing may not happen overnight, but with the right support, treatment, and self-awareness, you can work toward balance - both emotionally and hormonally.
Know that Your body and mind are on the same team. It's time to treat them like it.
Disclaimer: The information provided in this article is for general informational and educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or a qualified healthcare provider with any questions you may have regarding a medical condition.


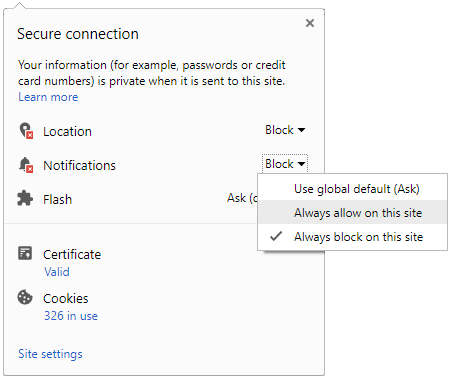
 Click it and Unblock the Notifications
Click it and Unblock the Notifications